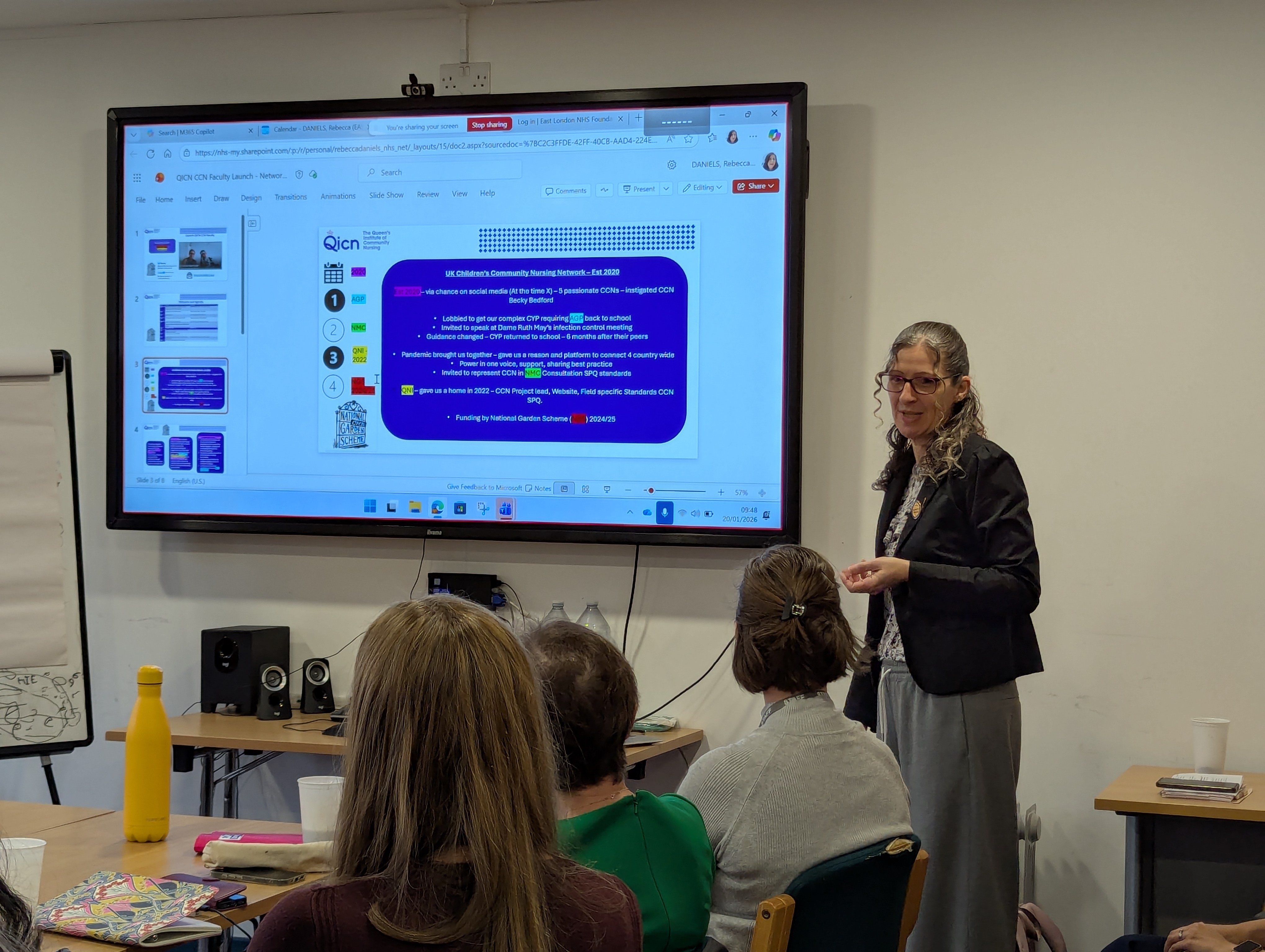
The event was opened by ELFT's own Rebecca Daniels BEM, CCN Network Lead at QICN and Community Children’s Matron who reflected on the journey of the UK Children’s Community Nursing Network. It was established in 2020 and has grown to 625 members with 27 meetings a year, providing a national platform for best practice, professional development and collective influence.
Rebecca also spoke about the development of the QICN Community Children’s Nursing Standards and the importance of supporting a skilled workforce equipped to care for babies, children and young people (BCYP) with complex health needs at home. She emphasised the network’s mission to ensure children “are supported to live their best possible life alongside their peers, with evidence-based care and the right skills available in the community.”
 Strengthening national foundations for CCN
Strengthening national foundations for CCN
Delegates heard from Steph Lawrence MBE, CEO of QICN, who outlined how the new Faculty will support a consistent, high-quality approach to community children’s nursing across the UK. The Faculty will sit within QICN’s wider remit to influence policy, develop standards, and champion innovation in community nursing.
Chief Executive, Lorraine Sunduza OBE, spoke about the importance of strong partnership working between QICN and provider organisations. She highlighted ELFT’s commitment to improving outcomes for children with complex needs and recognised the vital contribution of community nurses.
Spotlight on local practice and innovation
Local ELFT teams shared examples of quality improvement and new models of care being developed across Children and Young People’s Services (SCYPS)
1. Improving experience of care for young people with complex needs - getting transition right
Rebecca Daniels presented a QI project focused on supporting young people aged 7–18 with complex health needs through transition to adult health services. Key themes included the importance of respite, post-16 provision, changes in health outcomes after age 18, and the need for a more consistent, multi-agency approach. The project brings together community nursing, hospital transition teams, hospice partners and an ICB QI coach to strengthen preparation for adulthood, with measures including universal care plans, legal guardianship awareness and MDT transition templates.
2. Redesigning caseload management and developing nursing pathways
Teams presented learning from work underway to redesign caseloads within financial pressures, improving efficiency while maintaining safety and quality. This includes the creation of a Single Point Access referral form, a Triage Assessment Team, and six new nursing pathways covering short-term, acute, long-term conditions, complex disabilities, palliative and end-of-life care. The new model supports earlier identification of needs, streamlined MDT input, and more outcome-focused care planning.
 3. Specialist Practitioner Qualification (SPQ) learning in practice - Community Children’s Asthma Team
3. Specialist Practitioner Qualification (SPQ) learning in practice - Community Children’s Asthma Team
The Children’s Community Asthma Team shared how learning from the CCN SPQ programme is strengthening clinical practice, including risk stratification, leadership skills, transition planning and independent non-medical prescribing. The team demonstrated the impact of their work, including reducing hospital attendances, supporting self-management, and improving school attendance for children with asthma.
A shared vision for the future
Closing the event, QICN and ELFT colleagues reflected on the importance of growing and sustaining the CCN workforce through professional development, shared standards and strong national collaboration. The new Faculty will provide a home for this work, aligning education, innovation, quality improvement and policy influence to support children, young people and families across the UK.
The launch marks a significant milestone in strengthening the visibility, capability and voice of Community Children’s Nursing, ensuring that children with complex needs receive high-quality, compassionate care closer to home.
