What are Medically Unexplained Symptoms / Bodily Distress Disorder?
MUS/BDD refers to persistent bodily complaints for which adequate examination (including investigations) does not reveal any specified pathology. MUS/BDD is the term used to address disorders where physical symptoms have no medical explanation.
What is the Bodily Distress Disorder Service?
One-Stop-Shop
The Bodily Distress Disorder (BDD) Wellbeing Service offers a “One-Stop-Shop” service with a choice of group treatments – Meditation Based Stress Reduction (MBSR) and Strategies for Healthy Living Group (SHLG), a form of Body- Oriented Therapy.
These targeted group therapies have been developed and evaluated through research to improve enduring physical symptoms, working with and through embodiment. The focus is on improving physical, mental and emotional wellbeing.
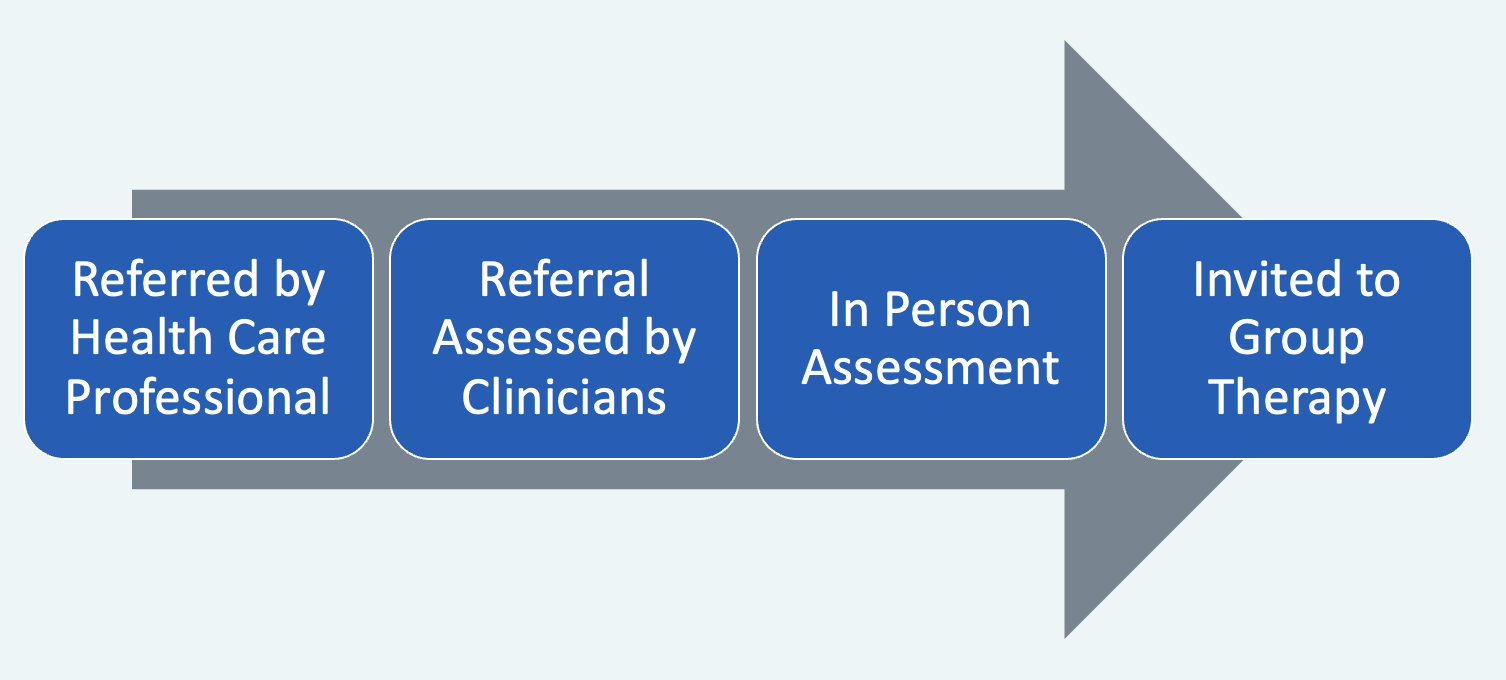
Referral Pathway